Home
Why Choose Us
Meet Our Doctors
Procedures
Cataract Procedures
Refractive Procedures
Cosmetic Procedures
Diabetes Eye Management
Pterygium Procedure
Other Procedures
Testimonials
Media
Cataract Procedures
Cataract Surgery
Cataract surgery is a procedure that replaces a cloudy lens in the eye with a clear artificial lens. It's the most common surgical procedure in the world.
Advanced Cataract Surgery
Advanced cataract surgery is a modern procedure that replaces a clouded natural lens with an intraocular lens (IOL). Using laser-assisted techniques.

Refractive Procedures

Cosmetic Procedures

Diabetes Eye Management

Other Procedures

Providing Exceptional
Eye Care in Los Angeles
When Your Eyesight is at its Best, Everything Becomes Clearer — Literally and Figuratively.

Diabetic Retinopathy
Diabetic retinopathy affects the retina, the part of your eye responsible for capturing light and creating images. High blood sugar levels damage the blood vessels in your eyes, leading to this condition.
Early intervention is crucial for managing this condition, as it can result in severe vision loss if left untreated. Additionally, regular eye exams and proper diabetes management can significantly improve quality of life.
What You Need to Know
Dr. Carlos Montoya and the team at St. Lucia Eye Center specialize in treating diabetic retinopathy. Using advanced treatments, we offer personalized care to help protect your vision.
Dr. Montoya Offers Tailored Treatments Based on Each Patient’s Needs Using the Latest Technologies to Preserve Vision
Benefits
- Prevents further damage to the retina
- Can improve vision or halt deterioration
- Personalized treatment plans
- Early detection leads to better outcomes
- Minimizes the risk of severe complications like blindness
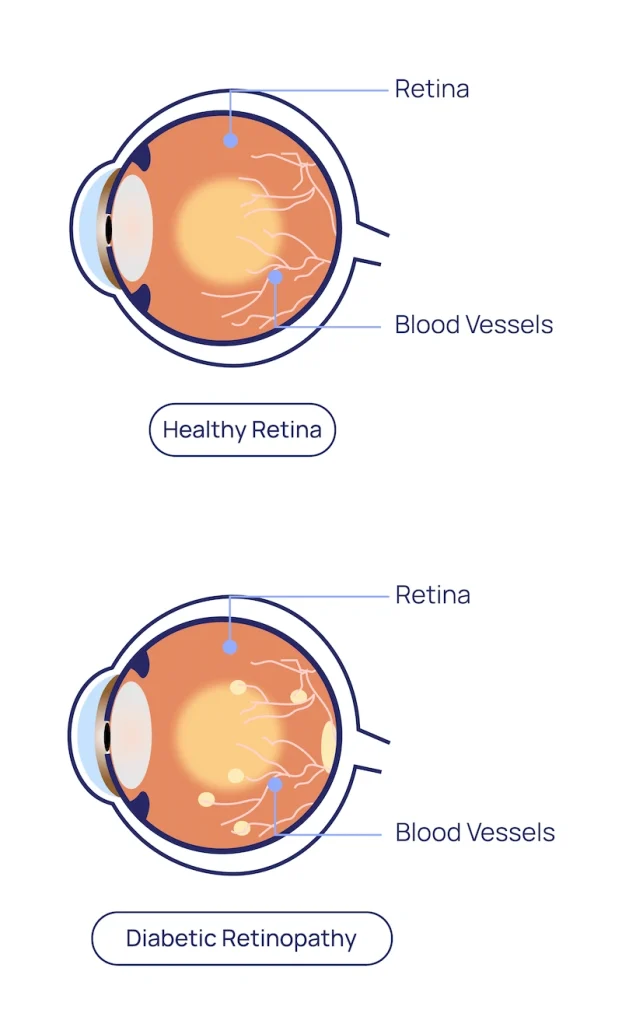
What is Diabetic Retinopathy?
Diabetic retinopathy occurs when high blood sugar damages the blood vessels in the retina. If left untreated, it can lead to blindness. However, early diagnosis and treatment can significantly reduce or prevent the risk of severe vision loss.
Symptoms
- Blurry or distorted vision
- Dark spots or floaters
- Trouble seeing at night
- Sudden vision loss (in advanced stages)
Given that early stages of this condition often have no symptoms, yearly comprehensive eye exams are crucial.
Symptoms
- Blurry or distorted vision
- Dark spots or floaters
- Trouble seeing at night
- Sudden vision loss (in advanced stages)
Given that early stages of this condition often have no symptoms, yearly comprehensive eye exams are crucial.
Types of Diabetic Retinopathy
Non-Proliferative Diabetic Retinopathy (NPDR)
In the early stage, blood vessels in the retina may swell, leak fluid, or become blocked. As a result, treatment primarily focuses on controlling blood sugar levels and preventing further progression of the condition.
Proliferative Diabetic Retinopathy (PDR)
In this advanced stage, abnormal blood vessels grow in the retina, which can lead to bleeding, retinal detachment, and severe vision loss. Therefore, timely treatment is essential to prevent further complications and preserve vision.
Causes of Diabetic Retinopathy
High Blood Sugar (Hyperglycemia)
Chronic hyperglycemia damages the small blood vessels in the retina, leading to leaks, weakness, or abnormal dilation.
Uncontrolled Diabetes
Poor management of blood sugar accelerates retinal blood vessel damage, ultimately causing vision loss.
Hypertension (High Blood Pressure)
Hypertension can contribute to an increased risk of blood vessel damage in the retina.
High Cholesterol
High cholesterol frequently contributes to fatty deposits in the retina, thus worsening damage.
Kidney Disease
Poor kidney function frequently correlates with worsening eye complications, which underscores the importance of managing both conditions.
Smoking
Smoking impairs the oxygen supply to the retina, therefore worsening the damage.

We Believe That Everyone Deserves to Enjoy Life With Clear Vision
Dr. Carlos Montoya and the team at St. Lucia Eye Center offer personalized care to help you manage diabetic retinopathy and maintain your vision. Don’t wait—schedule a comprehensive eye exam and take the first step toward protecting your sight.
How is Diabetic Retinopathy Diagnosed?
At St. Lucia Eye Center, we use advanced diagnostic tools to detect diabetic retinopathy in its earliest stages. With early care, most patients can protect their vision and significantly prevent severe complications.
Anti-VEGF Injections
Medications to reduce swelling and stop abnormal blood vessel growth.
Laser Therapy (PRP)
A laser treatment to seal leaking blood vessels and reduce the risk of further damage.
Vitrectomy
Surgical procedure to remove blood and scar tissue from the eye and repair retinal detachment in advanced cases.
Diabetic retinopathy is the leading cause of vision loss in people with diabetes. However, with proper diabetes management and regular eye care, you can significantly reduce your risk of serious complications.

When Do You Need Treatment?
Surgery may be required if you have advanced diabetic retinopathy, particularly if complications such as retinal detachment or severe bleeding occur. In such cases, specialized surgical procedures may be necessary to preserve or restore vision.
Are you a Candidate?
- People with diabetes (Type 1 or Type 2)
- Individuals experiencing vision changes due to high blood sugar
- Those with a family history of diabetic retinopathy
Timing
Early detection is crucial. As a result, the sooner treatment begins, the more likely it is that vision loss can be prevented.
Driving Requirements
Vision may be impacted in advanced stages. As a result, you may require assistance with driving.
Scheduling
Regular eye exams are essential for those with diabetes since they help detect any changes in the retina before they cause significant problems.
What else you should know
Understanding Diabetic Retinopathy
Diabetic retinopathy is a progressive condition that can be controlled effectively with proper treatment and careful management of diabetes. In addition, consistent monitoring helps avoid severe complications and ensures the preservation of vision.
Early Detection Saves Sight
Regular eye exams are the key to catching diabetic retinopathy in its earliest stages.
Managing Diabetes Reduces Risk
Maintaining blood sugar levels in control is essential for preventing or slowing the progression.
Vision Recovery
Early treatments, such as injections and laser therapy, can help stop the progression and restore vision in some cases.